Mental Health Help and Resources
Table of Contents:
- Suicide Prevention
- Dealing with Stress
- Avoiding or Coping with Depression During the Holidays (and beyond)
Suicide Prevention
Mental health and well-being is no different than physical health and well-being. Any one of us is subject to experiencing some form of mental health issue at some time in our life; and in most cases, afflictions are treatable and likely can be overcome with proper medical attention. And, like physical health concerns, left untreated, mental health conditions can become critical and life-threatening.
It is time we start the conversation about mental health and suicide, erase the stigma, and begin to help each other. Together, we can increase mental health and wellness, and prevent suicide.
"If a friend or a member of our family breaks their arm, we ask them what happened; maybe sign their cast, and joke with them about it. If someone we love comes down with a virus – whether something simple like a cold, or more serious – we encourage them to seek medical attention and ask how we can help. But if someone we know is struggling with a mental health concern, we hesitate . . . afraid to bring it up at all, much less offer any advice or assistance.
Why? Many times, it is because we do not know what to say or how to help. Plus, no one wants to 'accuse' someone of being crazy."
- Susann Mikkelson
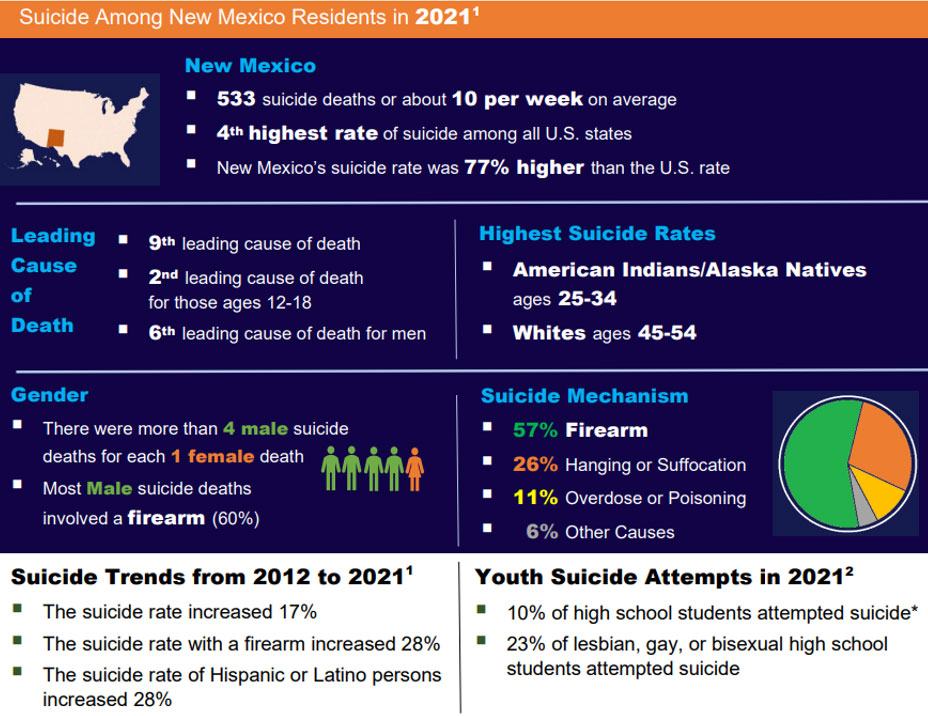
New Mexico reported 533 deaths by suicide in 2021, giving us the 4th highest rate of suicide in the United States. We know that this number is probably low; it is likely there were more suicides that went unreported as such, for various reasons.
Susann Mikkelson is a certified trainer in QPR. If you, your group, organization or business would like to offer a QPR Training, please contact the NMSU Guadalupe County Extension Office at 575-462-3652 or guadalupe@nmsu.edu.
Let’s Arm Ourselves with Awareness
Rural residents coping with mental health concerns face important barriers to treatment and relief. Among those barriers is the lack of access – or perceived lack of access - to treatment, the cost of treatment, and the sociocultural factors that increase the stigma around mental illness and what it means to seek help. This includes a culture of embarrassment – being afraid to be seen visiting the facility of a mental health provider; a culture of stoicism – being too proud or “tough” to seek treatment, which is often particularly an issue for males, and a culture of humility – being taught to not talk publicly about your problems.
Suicide has far and deep-reaching impacts
A study from the University of Kentucky found that, in addition to the direct loss of a life, suicide has the following additional impacts:
- An average of 135 people are exposed to a single death by suicide – this is the number of lives touched by one death
- 53 people will have a short disruption in life as a result of that one death – this may be co-workers or classmates, friends and acquaintances, emergency responders who responded to the crisis, and of course, family
- 25 people will have a major life disruption – this is the number of people whose lives will be changed for the long-term from one death by suicide
- On average, one suicide death will have devastating effects on 11 people – permanently altering their lives and often leading to more mental health concerns.
Important Resources
NM Crisis Access Line
1-855-NMCRISIS (662-7474)
If you or a loved one is experiencing any kind of emotional crisis, mental health, or substance use concern, you can find help 24 hours a day, seven days a week, by calling the New Mexico Crisis and Access Line or Peer-to-Peer Warmline.
nmcrisisline.com
National Suicide Prevention Lifeline
1-800-273-TALK (8255)
The National Suicide Prevention Lifeline is a 24-hour, toll-free, confidential suicide prevention hotline available to anyone in suicidal crisis or emotional distress. Your call is routed to the nearest crisis center in our national network of more than 150 crisis centers. The lifeline's national network of local crisis centers provides crisis counseling and mental health referrals day and night.
- Guadalupe County Health Council – 575-472-4567, or https://sharenm.org/guadalupe-county-health-council/
- Here To Help NM - https://www.nmflb.org/Here-To-Help-NM
- AgWell - https://rmfu.org/ or https://agwell.org/
- CHESS Health Connections App – https://chess.health/connections-app/
- 988 Suicide & Crisis Lifeline – https://988lifeline.org/
- 988 suicide & Crisis Lifeline Chat & Text: https://chat.988lifeline.org/
- NAMI-New Mexico - https://naminewmexico.org/resources/
- Blissful Minds New Mexico - https://blissfulnm.com/
- List of Therapists in New Mexico who accept Medicaid: https://zencare.co/new-mexico/medicaid
If it’s not a crisis, call a warmline or visit the WarmLines website. When you need someone to listen: Peer2Peer Regional Warmline: 1-833-626-1490
Guadalupe County Hospital: 575-472-3417
Sunrise Medical Clinic: 575-472-4311
Professional Counseling Associates of New Mexico: 575-472-5383
Team Builders: 575-472-0745
New Mexico Behavioral Health: 575-472-3068
Evidence-based research tells us that talking about suicide and mental health is one of the best ways to encourage treatment and prevent suicide. The more we learn, the more we share our caring compassion with others, the more we can avert suicide attempts that can alter the person’s life for a period of time or permanently, and the more we can prevent the tragedy of suicide.
Thanks to highly increased public awareness and resulting policy change, there are now many more options for anyone seeking assistance with a mental health crisis or concern, even those of us living in rural communities. These options are accessible from remote locations, and many are completely anonymous, if that is an important factor for anyone seeking assistance.
Some of these services include programs that help us learn more about how we, as average citizens, can be a part of the solution to this major health concern in our communities. Consult with the Guadalupe County Health Council for more information on local resources, or reach out online to some of the many services listed in this article for help. You do not have to be in crisis to reach out to these services – you could reach out to learn more about how you can help someone else, reach out on their behalf and help connect them, or just get further information in general.
QPR (Question, Persuade, and Refer) Gatekeeper Training is one training program for anyone and everyone that provides a basic understanding of and training on how each of us, as common citizens, can help be a part of mental health treatment and suicide prevention. QPR is to suicide prevention what CPR is to life-saving intervention for someone experiencing a heart attack or similar event. QPR will help each of us, as family members, friends, colleagues, teachers and care providers, or even just strangers passing on the street become “gatekeepers” and teach us how to help be the bridge between a person in crisis and the professional help they need to come out of that crisis in a healthy, thriving way.
Let’s start the conversation. Let’s help keep each other safe, healthy and happy – physically and mentally.
Sources for this article:
QPR Institute - https://qprinstitute.com/
CDC Suicide in Rural America
- https://www.cdc.gov/rural-health/php/policy-briefs/suicide-policy-brief.html
- https://www.cdc.gov/suicide/facts/
Share New Mexico – https://sharenm.org/
Download a PDF copy of this resource.
Dealing with Stress
The holiday season is coming, and with it come many feelings and emotions – warm thoughts of time with family and friends, gift giving and receiving, holiday activities and celebrations, from faith-based events to family gatherings, to shopping. For many, the holiday season can also be a stressful time, and for many, it can also conjure memories of loss, sadness, and loneliness, and can trigger or worsen depression. This month, we will look at stress and stress management. Please watch for the November article on Depression.
Stress, when not addressed, can lead to more serious, longer-term problems. When we are not addressing our needs for mental health and wellness, the results are actions and feelings that impact our interactions with others, our ability to function in our jobs and life. Over time, stress can affect our physical health as well as our mental health. Whether the coming holidays are bringing angst and stress, or there are other reasons for your feelings, understanding and addressing our stressors is important to our overall well-being.
What is Stress?
Stress can come in various forms and have different impacts. Three major classifications of stress include
- acute – highly intense stress for a short period of time,
- chronic – constantly present and difficult to avoid pressures and circumstances, and
- traumatic – usually from one or more unexpected and shocking experiences that bring immediate or long-term consequences often outside your control.
Psychologically, stress is the perception that your circumstances have exceeded your capacity to cope (creating a threat to your being). Physiologically (regarding the internal physical functioning of the body), stress is a state of internal imbalance where there is an over activation of the fight or flight response.
Signs of Stress
Some signs that stress is impacting you or someone in your life:
- Physical Signs
- Fatigue
- Digestive symptoms (upset stomach, heartburn, and related)
- Heart problems
- Insomnia
- Frequent headaches
- Random body aches
- Triggering of chronic and other health problems
- Emotional Signs
- Sadness
- Anger
- Anxiety
- Loss of sense of humor
- Behavioral Signs
- Irritability
- Short or quick temper
- Unusually quiet or isolating oneself
- Unusual effort to be portray happiness or jubilance
- Increased use of alcohol and drugs
- Cognitive Signs
- Lack of concentration
- Memory thoughts
- Difficulty with decisions
- Change to Self-Worth
- Feeling like a failure
- Feeling overwhelmed
- Feeling alone or lonely
- Self-deprecating statements or thoughts
Addressing the Issue and Dealing with Stress
The first important step to lowering stress and regaining wellness is recognizing that there is an issue. But it is important to take that a step further – to actually identifying the core issue or issues causing the stress, and working to address them and how they impact our life.
Factors of stress exist for all of us. Each of us handles those various factors differently, depending on our temperament, their life experiences, and other circumstances. We should not minimize a stress factor for us or for someone else. Some stress factors can be minimized or eliminated. Other stressors may be ongoing, in which case we need to find ways to manage and minimize the stress is causes us.
Tips and Ideas to Identify and Minimize Stressors
- Speak with someone you trust – a friend or family member, a member of clergy, or a counselor – who can help you sort through your stressors and how to approach them differently
- Keep a journal and get your feelings out; sometimes hearing or reading our thoughts and feelings helps us process them more objectively
- Build in quiet time for yourself, even if just a few minutes, every day
- Make a concerted effort to plan and make decisions that will avoid stressors or make them less stressful
- Build in time for activities that bring you joy and peace, and take your mind off of your worries; examples might include:
- Exercise such as walking or going for a bike ride
- Go for a drive (safely)
- Spend time with people you love and care about
- Have a game night or movie night with friends
- Give time to others in need
- Spend time with beloved pets or volunteer to help at the animal shelter
Addressing and resolving stress is about formulating a plan that works for us, implementing that plan, and adapting over time, as we learn what works for us and find new ways of managing and minimizing stress.
Ignoring stress will often lead to more serious problems. At a minimum, it will spread to those around us, those we love. None of us wants to cause stress to our loved ones. Long-term, ignoring or minimizing our stress will inevitably lead to other, more serious issues, both mental health and physical health related.
We should never feel embarrassed or ashamed about taking care of our mental well-being. Just as we sometimes need to involve outside experts – medical professionals – in our physical health and well-being, we also sometimes need to bring in outside resources to manage our own mental health and well-being. It is not shameful to ask for help; rather, it is brave, courageous and smart.
Stay SMARRTT Guadalupe County
– Strive to Maintain A Robust, Resilient and Tranquil Trek
Sources for this article:
- NMSU College of ACES https://nmhealthwellness.nmsu.edu/more/stressmanagement.html
https://nmhealthwellness.nmsu.edu/index.html
- NM Farm and Ranch Stress Assistance Network https://portal.nifa.usda.gov/web/crisprojectpages/1027236-new-mexico-farm-and-ranch-stress-assistance-network.html
- Other NMSU publications and NMDA resources
https://nmdeptag.nmsu.edu/mental-health-resources.html
Susann Mikkelson is a trained PEARLS (Program Encouraging Active, Rewarding LiveS) Coach, trained in other mental health and wellness programming, and a certified QPR (Question, Persuade, Refer) Suicide Prevention Program trainer. If you are interested in PEARLS or other mental health and wellness programming, or your group, organization or business would like to offer a QPR Training, please contact the NMSU Guadalupe County Extension Office at 575-462-3652 or susannm@nmsu.edu.
Avoiding or Coping with Depression During the Holidays (and beyond)
The holiday season upon us, bringing with it many feelings and emotions – warm thoughts of time with family and friends, gift giving and receiving, holiday activities and celebrations – from family gatherings to community events, to shopping. For many, the holiday season can also be a stressful time, and – also for many – it can conjure up memories of loss, sadness, and loneliness, and can trigger or worsen depression. In this edition, we will take a closer look at how to avoid becoming depressed or cope with symptoms of depression. Please see our previous articles in September and October issues of The Communicator regarding other mental health and wellness topics.
If we ignore a physical health concern, it will worsen and impact us in bigger ways. Similarly, stress and depression, left untreated, will inevitably lead to more serious problems. When we don’t address our mental health and wellness needs, the results are actions and feelings that impact our daily lives – our ability to find pleasure in routine activities we have enjoyed in the past, interactions with loved ones, friends and others, our ability to function in our jobs and life. In fact, over time, stress and depression can affect our physical health, as well. Whether the coming holidays are bringing sadness, angst and depression, or you have other reasons for your feelings, understanding and addressing signs and symptoms of depression are critical to not only your mental well-being, but also your physical health and wellness.
Signs and Symptoms of Depression
Everyone feels sad or ‘low’ sometimes, but these feelings usually pass. Depression is different. It can cause symptoms, sometimes severe, that overtake all or most ‘normal’ feelings, thoughts and daily actions, including basic activities such as eating, sleeping and concentrating on work or school. There are several types of depression; major depression, persistent depressive disorder, seasonal affective disorder or clinical depression, are some examples.
Depression can affect anyone regardless of age, gender, race or ethnicity, culture, level of income or education. Research suggests that biological, environmental, genetic and psychological factors can each effect depression.
In addition, depression can co-occur with other mental or physical disorders. Chronic illnesses such as diabetes, cancer, heart disease and chronic pain disorders can trigger depression, and in turn, depression can make the symptoms of these illnesses worse. Sometimes, even medications taken for an illness can cause side effects that contribute to symptoms of depression.
If you are feeling symptoms that you think might be depression, consulting your general practitioner might be the best place to start with getting the care you need, since they are aware of your overall health and wellbeing.
Signs you may be depressed:
- Persistent or extreme feelings of -
- sadness, anxiousness, or apathy (emptiness, lack of care)
- hopelessness, helplessness, or pessimism
- irritability, frustration, restlessness or anger
- Loss of sense of humor
- A significant change in mood or behavior, including those listed above, and
- unusual irritability or a quick temper
- unusually quiet or isolating oneself
- increased use of alcohol and/or drugs
- unusual effort to portray happiness or jubilance
- increased impulsiveness and/or engagement in new, high-risk activities
- an unusually flippant or apathetic attitude
- physical and cognitive changes, such as -
- lack of ability to concentrate and remember
- feeling fatigued and drained, lacking motivation and enthusiasm
- difficulty or inability to make decisions
- difficulty sleeping or major changes in sleep patterns
- significant changes in appetite, and associated weight gain or loss
- new or unusual aches and pains, including frequent, unexplained headaches, muscle aches, and cramps
- digestive changes and issues
- change to self-worth, including -
- noticeable and new statements and thoughts of self-deprecation
- becoming easily overwhelmed
- expressing signs of loneliness
Addressing symptoms of and treating depression
If you are feeling or noticing any of these signs or symptoms, it is best to seek treatment as quickly as possible. The sooner you address your feeling and other symptoms, the better your chances of recovery and return to a well state of being. The longer you wait, the more likely symptoms will increase and possibly become serious, causing problems in your professional and personal life, and raising other health problems.
Formal treatment for depression may include various forms of therapy, medication, changes of lifestyle and natural remedies. This article and its tips are NOT intended to replace appropriate treatment by a professional provider. Seeking external support for your health and wellness concerns is essential to recovering and leading a healthy life.
Symptoms of depression can vary widely from one person to another. Your primary healthcare provider may be the best person for you to start with when seeking help and getting the care you need. If you do not have a primary provider, do not have access to your provider for some reason, or if you are uncomfortable raising these concerns with your provider, there are some resources listed below that might help you get on a path to healing and recovery.
However, here are a few tips that may help you manage your mental well-being and keep depression from setting in and taking over:
- getting at least 30 minutes of some form of physical activity daily;
- regulating your body’s cycles with regular meal times and regular sleeping patterns, to the best of your ability;
- develop habits of positive activities and practices that enhance your mood and spirits – these can be simple actions that do not require a great effort, such as:
- keep a journal or record messages to yourself, and make sure to document positive aspects of your daily life, not just negative aspects;
- be mindful of your ‘inner voice’ to yourself and how you treat yourself - focus on giving yourself grace and forgiveness, celebrate (honor) the positive steps you take, even if small, toward your goals and well-being, and be patient with yourself;
- find activities that bring you joy or pleasure, such as looking at pictures of people, animals or beautiful scenery, or listening to upbeat or relaxing music, and engage in these activities regularly;
- attend church and/or other group activities which help you interact with other people in a positive environment;
- embark on or study a new hobby or interest;
- avoid activities and habits that noticeably bring sadness or dampen your mood, including consuming drugs or alcohol.
Sources for this article:
National Institute of Mental Health Suicide in Rural America
Susann Mikkelson is a certified trainer in QPR and also offers trainings on stress, mindfulness and other wellness programming. If you, your group, organization or business would like to offer a QPR Training or other program, please contact the NMSU Guadalupe County Extension Office at 575-472-3652 or guadalupe@nmsu.edu.